Why Your Body Needs More Than Time to Heal
Your Body Is Healing. Here's How to Support It from the Inside Out, Perfect for post-surgery, new moms, or catheter users.
Whether you're recovering from surgery, navigating new motherhood, or managing a catheter, your body is working hard to repair itself. Healing isn't automatic; it requires the right fuel and support to prevent complications and regain strength.
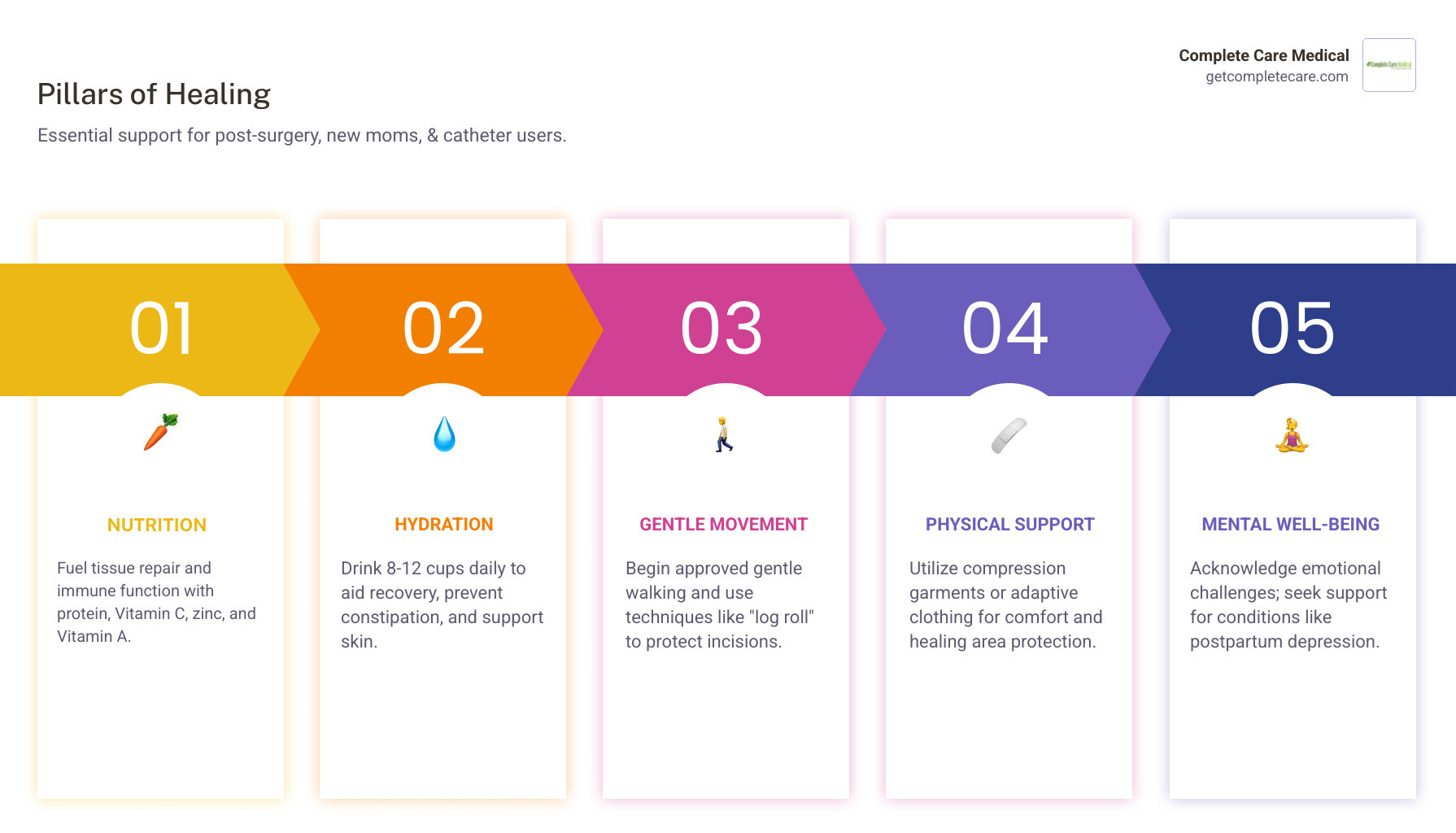
Quick Guide: How to Support Your Body's Healing
- Nutrition: Prioritize protein (1.5-2.0g per kg body weight), Vitamin C (1,000-2,000mg daily), zinc, and Vitamin A.
- Hydration: Drink 8-12 cups of fluid daily to flush anesthesia, prevent constipation, and support skin health.
- Movement: Start gentle walking when approved and use safe techniques like the "log roll" to protect incisions.
- Physical Support: Use compression garments or adaptive clothing to protect healing areas.
- Mental Health: Acknowledge emotional challenges and seek support, especially given the 15% higher risk of postpartum depression after unplanned C-sections.
The first six to eight weeks are critical. Postpartum constipation affects 52% of new moms, and surgical patients are four times more likely to develop blood clots without proper movement. Your nutritional needs can increase by 50% for complex wounds, yet guidance is often minimal.
This guide details what your body needs to heal faster and reduce complications, from key nutrients to practical daily strategies.
Your Body Is Healing. Here's How to Support It from the Inside Out.
Fueling Your Recovery: The Role of Nutrition and Hydration
During recovery, your body needs quality materials to rebuild. Without proper nutrition, healing slows, infection risk climbs, and fatigue persists.
Protein is your healing MVP, with needs skyrocketing to 1.5-2.0g per kg of body weight daily to repair tissue and muscle. Good sources include lean meats, fish, eggs, dairy, beans, and nuts. Protein shakes are great when chewing is difficult.
Complex carbs (brown rice, oats) provide sustained energy, while healthy fats (avocados, nuts, fatty fish) reduce inflammation.

Key vitamins and minerals also accelerate healing. Vitamin C (citrus, berries) is crucial for collagen production. Zinc (meats, beans) supports tissue repair. Vitamin A (leafy greens, carrots) aids cell growth, but check with your doctor first. If you've lost blood, iron (red meat, poultry) is vital for oxygen transport.
Water is the unsung hero of recovery, flushing anesthesia and preventing constipation. Aim for 8-12 glasses of fluid daily. Fiber is also essential; get both soluble (oats, apples) and insoluble (brown rice, leafy greens) types to aid digestion. Scientific research on fiber confirms its importance for digestive health.
Top healing foods include lean proteins, colorful fruits and vegetables, healthy fats, whole grains, and bone broth, which is rich in collagen.
Practical Eating Strategies When Appetite and Energy Are Low
When pain or fatigue makes eating feel impossible, these strategies help:
- Eat small, frequent meals to maintain steady energy.
- Accept smoothies for an easy, nutrient-dense option.
- Sip bone broth for hydration and collagen.
- Manage nausea with bland foods like toast or ginger tea.
- Relieve constipation with fiber, fluids, and gentle movement. Ask your doctor about stool softeners.
- Ask for help with meals and groceries. Your job is to heal.
Special Considerations for New Moms and Catheter Users
New mothers and catheter users face unique recovery challenges.
For new moms, nutritional needs are high, especially if breastfeeding. C-section recovery is major surgery (4-8 weeks). Pain management is key; consult your doctor about safe medications and refer to ACOG's resources on postpartum pain management. C-section moms face higher risks of constipation and blood clots, making hydration, fiber, and gentle walking critical. Be aware of your emotional well-being; unplanned C-sections carry a 15% higher risk of postpartum depression.
If you're using a catheter, focus on preventing UTIs. Hydration is paramount to flush the urinary system. Avoid bladder irritants like caffeine and alcohol. Prevent constipation, as a full bowel can press on the bladder. Proper hygiene and using the correct catheter are crucial for comfort. Our team at Complete Care Medical can help you get the right insurance-covered supplies.
Supporting Your Physical Recovery: Movement and Supportive Garments
Gentle movement, once approved, is vital. Early movement like short walks prevents blood clots and aids digestion. To protect abdominal incisions when getting out of bed, use the "log roll" technique: roll to your side, then use your arms to push up.

Supportive garments like abdominal binders reduce swelling and pressure on incisions. Adaptive clothing with high waistbands or easy closures (side-zippers, magnets) offers comfort and dignity. Choose soft, breathable fabrics like cotton to prevent chafing.
Nurturing Your Mind: The Psychological Side of Healing
Emotional health is inseparable from physical recovery. The stress of pain, fatigue, and loss of independence can lead to post-surgery depression and anxiety. Sleep deprivation worsens this, so it's normal to feel frustrated. Here’s how to nurture your mind:
- Prioritize rest. It's a medical necessity, not a luxury. Enlist help to get as much sleep as possible.
- Seek support. Lean on your partner, friends, and family. Join a support group or speak with a therapist if feelings of sadness or anxiety persist.
- Practice mindfulness. Gentle meditation, deep breathing, or even just listening to calming music can reduce stress and pain.
- Journal. Writing down your thoughts can help you process emotions and track your progress.
- Celebrate small victories. Acknowledging small steps—walking a bit further, showering alone—reminds you that healing is happening, even when it feels slow.